For couples struggling with infertility, the journey to parenthood can feel daunting. But advances in medical science have made it possible for many to experience the joy of having a child. One such groundbreaking procedure is Intracytoplasmic Sperm Injection (ICSI), a revolutionary technique designed to overcome severe male infertility.
In this blog, we’ll explore what Intracytoplasmic Sperm Injection (ICSI) is, how it works, its benefits, risks, success rates, and how it can change the lives of couples yearning for a family.
What is Intracytoplasmic Sperm Injection (ICSI)
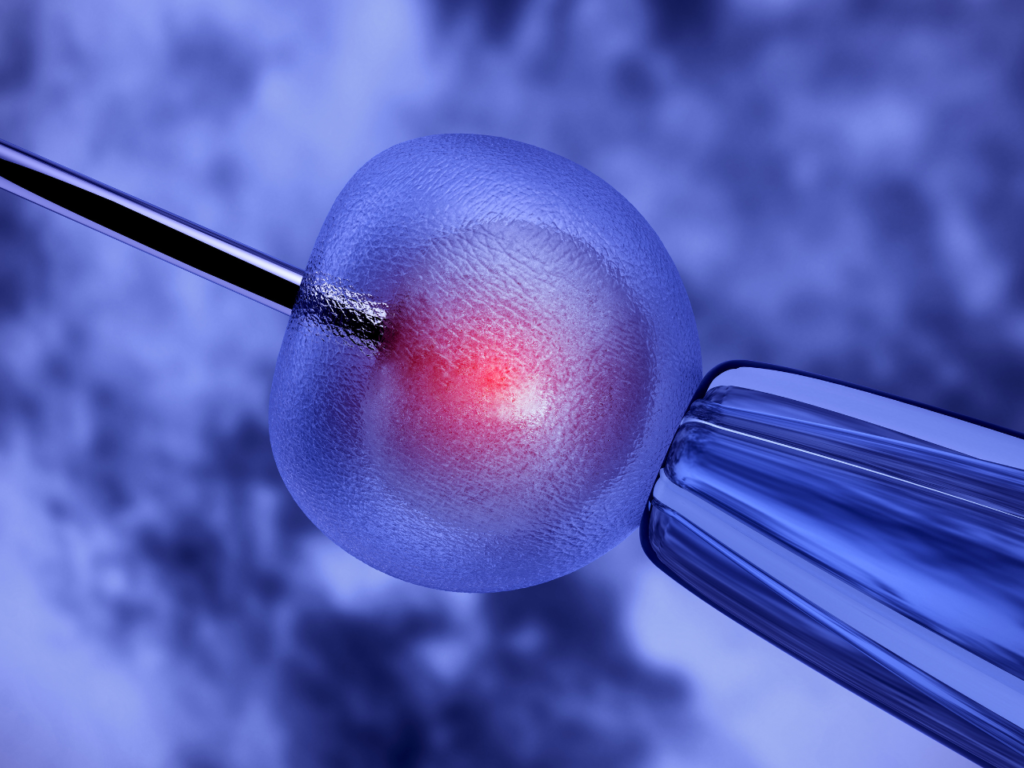
Intracytoplasmic Sperm Injection (ICSI) is an advanced fertility procedure where a single sperm is directly injected into an egg to achieve fertilization. It is a part of in-vitro fertilization (IVF) and is often recommended for couples dealing with male infertility factors such as:
- Low sperm count (oligospermia)
- Poor sperm motility (asthenozoospermia)
- Abnormal sperm morphology
- Previous failed fertilization in IVF cycles
Unlike traditional IVF, where thousands of sperm surround the egg in a petri dish hoping for natural fertilization, ICSI bypasses this process by injecting one selected sperm directly into the egg.
Who Needs Intracytoplasmic Sperm Injection (ICSI) ?
- Male Infertility:
ICSI is highly effective in cases of male infertility, particularly when sperm quality or count is extremely low. - Unexplained Infertility:
It is also beneficial for couples with unexplained infertility who haven’t had success with other treatments. - Failed IVF Attempts:
Couples who have had poor fertilization rates in previous IVF cycles often find success with ICSI. - Frozen Sperm Usage:
ICSI is ideal when using sperm from cryopreservation or a surgical sperm retrieval procedure like TESA (Testicular Sperm Aspiration) or MESA (Microsurgical Epididymal Sperm Aspiration).
Step-by-Step Process of Intracytoplasmic Sperm Injection (ICSI)
Ovarian Stimulation:
- The female partner receives medications to stimulate the ovaries to produce multiple eggs.
- These eggs are carefully monitored using ultrasound scans and blood tests.
- Egg Retrieval:
- Eggs are retrieved using a minimally invasive procedure called transvaginal ultrasound-guided aspiration.
- Sperm Collection:
- Sperm is collected from the male partner via ejaculation or surgical extraction (if necessary).
- The sperm is then prepared in a lab to select the healthiest one.
- Injection of Sperm into Egg:
- A skilled embryologist uses a fine glass needle to inject a single sperm into the center of each egg.
- This requires a high degree of precision and expertise.
- Fertilization and Embryo Development:
- Fertilized eggs are monitored for several days to ensure proper cell division and development.
- Healthy embryos are selected for transfer.
- Embryo Transfer:
- The best-quality embryo is transferred into the uterus, where it has the potential to implant and result in a pregnancy.
Benefits of (ICSI)
- Overcomes Severe Male Infertility: Even when only a few viable sperm are present, ICSI can make fertilization possible.
- High Fertilization Rates:The controlled process ensures a higher chance of fertilization compared to conventional IVF.E
- ffective for Frozen Sperm:Cryopreserved sperm or surgically retrieved sperm can be successfully used.
- Increases Pregnancy Chances:For couples who’ve experienced failed IVF cycles, ICSI improves their odds of success
Risks and Considerations
- Egg Damage:
- There’s a small chance the process of injecting sperm can damage the egg.
- Fertilization Failure:
- Despite precision, some eggs may not fertilize after injection.
- Embryo Quality:
- Not all fertilized eggs develop into healthy embryos.
- Genetic Concerns:
- In cases of male infertility due to genetic factors, the risk of passing these issues to offspring should be considered. Genetic testing is often recommended.
Success Rates of (ICSI)
The success of ICSI depends on several factors, including:
- The age of the female partner (younger eggs have higher success rates)
- The quality of sperm and eggs
- The skill of the embryologist
On average, ICSI results in fertilization in 50-80% of cases, with pregnancy rates ranging from 35-50% per cycle, depending on individual circumstances.
How to Prepare for ICSI
- Medical Evaluation:
- Both partners should undergo thorough fertility evaluations to determine the root cause of infertility.
- Healthy Lifestyle:
- Maintaining a balanced diet, reducing stress, and avoiding smoking or alcohol can improve treatment outcomes.
3.Open Communication:
Discuss your concerns, expectations, and questions with your fertility specialist to make informed decisions.
Conclusion
Intracytoplasmic Sperm Injection (ICSI) is a beacon of hope for couples battling infertility. Its ability to overcome severe male infertility and improve fertilization rates makes it a preferred choice for many. By understanding the procedure, its benefits, and its risks, you can take an informed step toward achieving your dream of parenthood.
This life-changing treatment, coupled with advancements in reproductive medicine, has brought the joy of parenthood to millions worldwide.
FAQs About ICSI
ICSI involves directly injecting a single sperm into an egg, while traditional IVF allows sperm to naturally fertilize the egg in a lab dish.
While ICSI is commonly used for male infertility, it’s also effective for unexplained infertility, previous failed IVF cycles, or when using frozen or surgically retrieved sperm.
ICSI has higher fertilization rates than conventional IVF, especially in cases of male infertility, but pregnancy success also depends on factors like egg quality and the woman’s age.
Risks include potential egg damage during injection, fertilization failure, and genetic concerns, particularly if male infertility is caused by genetic issues.
The ICSI procedure itself is quick, taking only a few minutes per egg, but the entire process from ovarian stimulation to embryo transfer spans about 2-3 weeks




